Abstract

Eltrombopag (EPAG) received FDA approval for treatment of refractory severe aplastic anemia (rSAA) in 2014, based on our phase I/II dose escalation trial of single agent EPAG at 50-150 mg daily over a period of 12 weeks (Olnes NEJM 2012; Desmond Blood 2014).
Two observations warranted further investigation of EPAG in this unique patient population. First, cell count kinetics and lack of acute toxicities suggested that extended administration of EPAG at a fixed dose of 150mg could speed and improve response rates. Second, 19% of patients developed new cytogenetic abnormalities on EPAG, raising concerns that EPAG might promote progression to MDS/AML.
We conducted a subsequent phase II study of EPAG given at a fixed daily dose of 150mg for 6 months in patients with rSAA (NCT01891994). Thirty-nine patients enrolled between July 2013 and April 2017. Primary endpoint was hematologic response at 6 months. Responding participants could continue EPAG treatment. Secondary endpoints included response at 3 months and the rate of clonal cytogenetic evolution.
Nineteen of 39 (49%) patients met criteria for hematologic response at 6 months. Of these, 5/19 (26%) patients would have been deemed non-responders at 3 months of treatment. EPAG was continued in 18 patients on the extension arm. EPAG was discontinued for robust response in 13/18 (72%) after a median duration of drug administration of 12 months (6-27.5 months). EPAG was re-initiated for relapse in 3/13 patients, and all 3 recovered response.
At median follow up of 6 months (range 2 - 39 m), 6/39 patients (15%) developed marrow cytogenetic abnormalities, a rate comparable to our previous cohort.
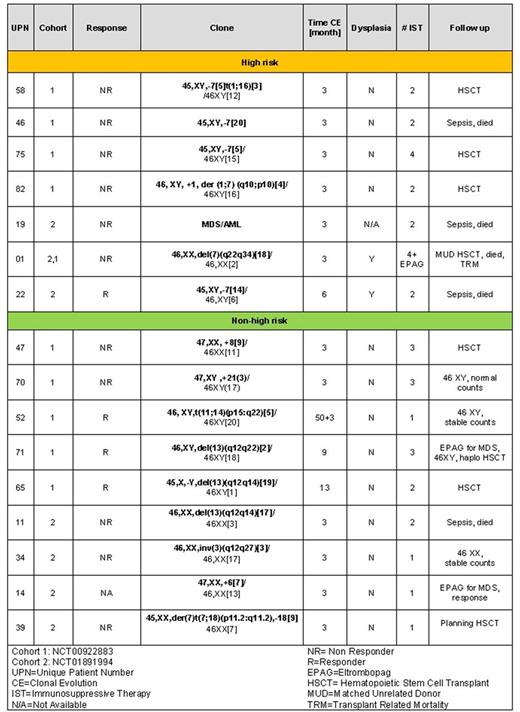
Given the similar rates of response and clonal evolution in our two consecutive studies, we analyzed the relationship between outcomes and cytogenetic progression for all patients (n=83) at up to 8 years of follow-up. Sixteen of 83 (18%) patients clonally evolved (Table 1). Clonal evolution was an early event after EPAG initiation. Evolution occurred within 6 months in 13/16 evolvers (81%), and in 6/6 evolvers with high risk chromosome 7 abnormalities (5/6 within 3 months). The frequency of high risk clonal evolution 24 months post intervention is comparable to historic controls with rSAA. However, direct temporal comparisons of evolution events are limited by differences in the sequence of cytogenetic tests. Non-chromosome 7 cytogenetic abnormalities were often transient, and not associated with dysplasia. Two evolvers continued EPAG off the rSAA protocol and cytogenetics normalized (UPN 71,14).
The acquisition and selection of somatic mutations, particularly of myeloid candidate genes recurrently mutated in MDS/AML, has been proposed to be an initiating step in clonal evolution. We performed whole exome sequencing (WES) on samples obtained pre-EPAG treatment and at the primary response endpoint and/or time of clonal evolution in 21 responding patients and in 11 patients with cytogenetic evolution. Candidate gene mutations were detected in patients who responded (6/21) and in those with cytogenetic evolution (4/11). Clonal hematopoiesis without an identifiable driver mutation was common. In post-EPAG samples, additional myeloid candidate gene somatic mutations were detected in 2 cytogenetic evolvers and in 4 responding patients, all at low variant allele frequencies (VAF) that were close to the 2.5% detection threshold. There was no significant change in VAF in either candidate or in non-candidate genes in responders and in cytogenetic evolvers. Only one early cytogenetic evolver (UPN 01) showed an expansion of mutated clones (SETBP1 and RUNX1), from VAF of 5% to 40%, when 80% of bone marrow metaphases showed chromosome 7q deletion.
In summary, extended administration of EPAG at a fixed dose of 150 mg daily for 6 instead of 3 months induces additional responses in a subgroup of patients with rSAA. After EPAG was discontinued, most patients maintained durable robust responses. The temporal relationship between clonal evolution and drug exposure suggests that in a subgroup of patients, EPAG may promote expansion of dormant pre-existing clones with an aberrant karyotype. No clinical or laboratory findings prior to therapy, including WES, predicted response or risk of clonal evolution. Careful monitoring of refSAA patients treated with EPAG is indicated, particularly in the first 6 months of treatment.
Winkler: Novartis/GSK to institute: Research Funding. Cooper: Novartis/GSK to institute: Research Funding. Townsley: Novartis/GSK to institute: Research Funding. Grasmeder: Novartis/GSK to institute: Research Funding. Young: Novartis/GSK to institute: Research Funding. Dunbar: Novartis/GSK to institute: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract